
In this four-part series, we explore the various challenges facing orphan medicines entering the European market and suggest solutions that can help improve patient access. In Part 3 of the series, we explore the challenges linked to generating economic evidence.
“It has been accepted that orphan medicinal products are not normal goods, but neither are they luxury goods that you can choose not to have. As a society, we do have an inclination to fund those most in need. Why this happens is still a matter of debate, but it has been shown that there is willingness to care for those more in need”, says Oriol de Sola-Morales, a former Director of a regional HTA Agency in Spain and founding member of the international body EUnetHTA2 in The European Journal of Health Economics (2019).
In this age of rampant innovation coupled with economic recession and increasing budget pressure, healthcare system affordability is more critical than ever, especially in an area with high price-per-treatment tags. The list of the most expensive drugs is now headed by advanced, potentially curative therapies that are administered once, and which often target rare diseases. Thus, there is a significant need to model the economic benefits of such high-cost medicines and demonstrate the overall economic value to payers and healthcare systems.
Despite a greater willingness to fund and award higher prices to orphan medicines, as shown in the quote above, pharmaceutical manufacturers still need to balance affordability by healthcare systems with the capacity to recoup investments made with a smaller target population and typically highly innovative technologies.
Where separate HTA processes exist and are already adapted to the orphan medicine reality, manufacturers should aim to meet the criteria and requirements for selection via these routes. Where this is not possible, manufacturers must navigate the regular frameworks and processes, and anticipate and overcome hurdles posed by payers. The disease knowledge and awareness and clinical evidence development challenges described in Parts 1 and 2 of this series combine to make economic modelling in rare diseases particularly difficult.
Challenges in generating economic evidence
Below, Calum Jones explains the challenges faced by health economists when looking to demonstrate the value of orphan medicines:
- If the natural history of the disease is poorly understood such that few, if any, previously published model structures can be leveraged, structural conceptualisation of the patient pathway will likely be intellectually demanding and require multiple assumptions. This may necessitate the development of a de novo Payers may struggle to accept this heightened uncertainty in the economic impact of the new orphan therapy.
- The core underlying clinical trial(s) for the new treatment may have several submission-undermining issues, including a limited duration (for what may be a chronic debilitating disease), the use of surrogate endpoints rather than true clinical outcomes, and small patient numbers leading to weakly powered trials with wide confidence intervals around estimated effect sizes.
- A heterogenous patient population can complicate the use of assumptions that apply to the whole patient cohort, e.g. identification of the minimum clinically meaningful time interval to detect differences between the new treatment and comparator (i.e. the model cycle length).
- Existing literature may provide little or no data on effective comparators for the new intervention nor on management costs for the rare disease.
- High prices for new rare disease treatments, a relative lack of standardisation in disease management, and substantial uncertainties in underlying effectiveness and cost data can often cause incremental cost effectiveness ratios to exceed commonly accepted thresholds.
Solutions to improve economic evidence generation for rare diseases
The benefits and costs associated with treating a rare disease often extend indirectly beyond the patient. Existing HTA processes infrequently consider indirect effects by default; however, manufacturers can aim to communicate significant socioeconomic benefits and costs linked to patients’ economic participation, and associated alleviation of the caregiver burden.2
Metrics for capturing humanistic and societal costs and benefits include patient quality of life, caregiver quality of life, loss of productivity (patient and caregiver), hours of formal and informal care provided, and loss of employment.
Patient registries and real-world data linked with country-relevant healthcare resource utilisation measures can also support the economic argument for a new orphan medicine where long-term data from clinical trials are often scant.
The disease pathway structure and/or accompanying assumptions for a rare disease can often be informed by previously published economic models in analogue or proxy disease areas. For example, while the evidence base for neurodegenerative disorders as a whole is growing, this is not true for distinct subsets of this disease area. Consequently, modelers exploring the cost-effectiveness of a new motor neurone disease treatment (compared to standard of care) may benefit from pragmatically leveraging previously published model structures and assumptions relating to Alzheimer’s or Huntington’s disease, while diligently outlining the inherent limitations of doing so.
Learnings taken from proxy diseases should generally be applied conservatively, with the conceptualised patient pathway and chosen model type always validated by key clinical experts experienced in the management of the rare disease in question. Rationales should be clearly stated and, if possible, referenced.
If you’d like to discuss these topics with us and would like to hear more about how we can help you overcome your current challenges in a rare disease area, please email info@mtechaccess.co.uk to arrange a meeting with one of our experts.
References:
- de Sola-Morales, O. Funding orphan medicinal products beyond price: sustaining an ecosystem. Eur J Health Econ. 2019;20:1283–1286.
- EunetHTA website. Available from: https://eunethta.eu/. Accessed on January 2021

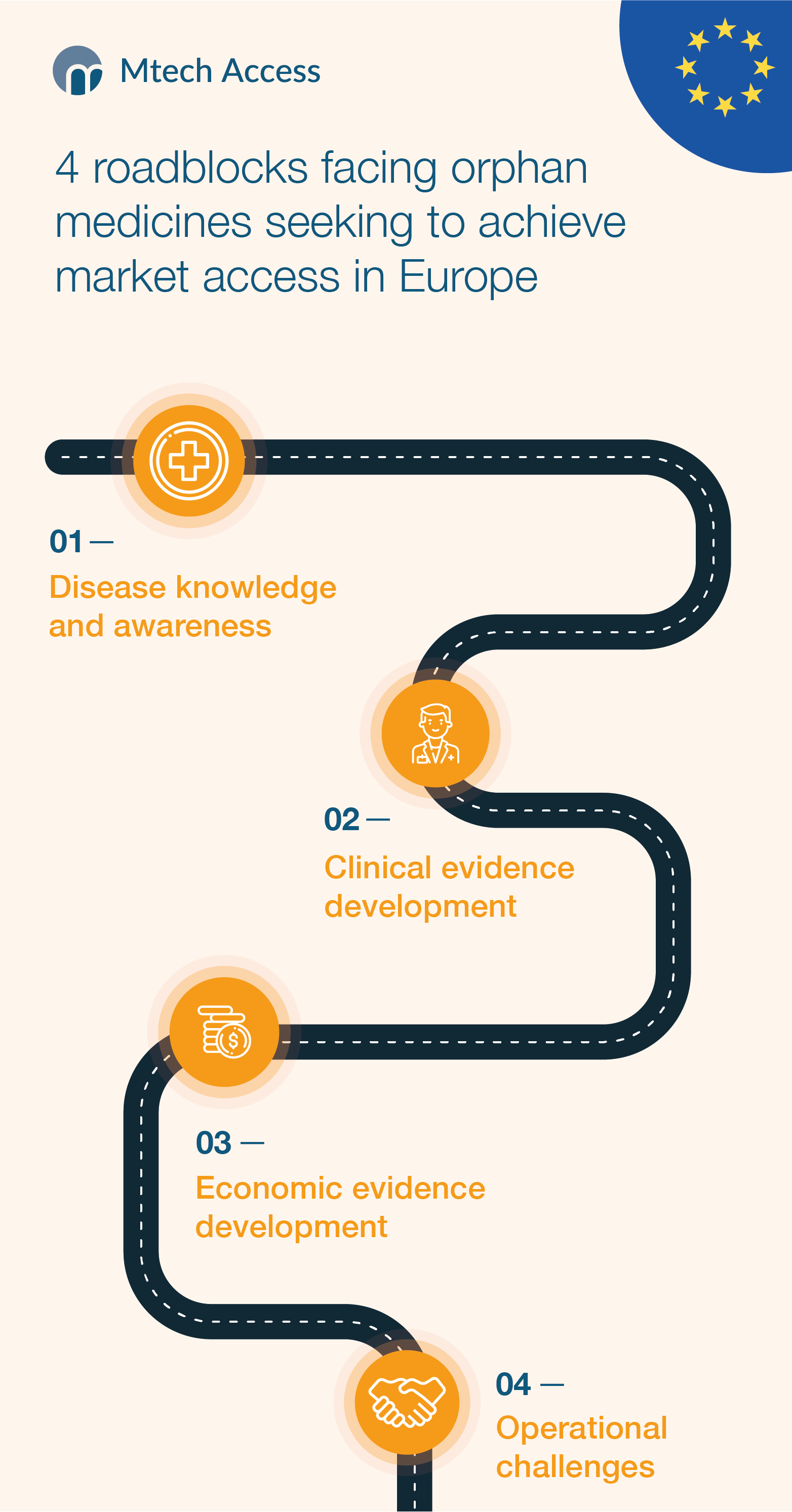





[…] Read Part 1: Disease knowledge and awareness Read Part 3: Economic evidence development […]
[…] Read Part 2: Clinical evidence development Read Part 3: Economic evidence development […]
[…] Read Part 1: Disease knowledge and awareness Read Part 2: Clinical evidence development Read Part 3: Economic evidence development […]