
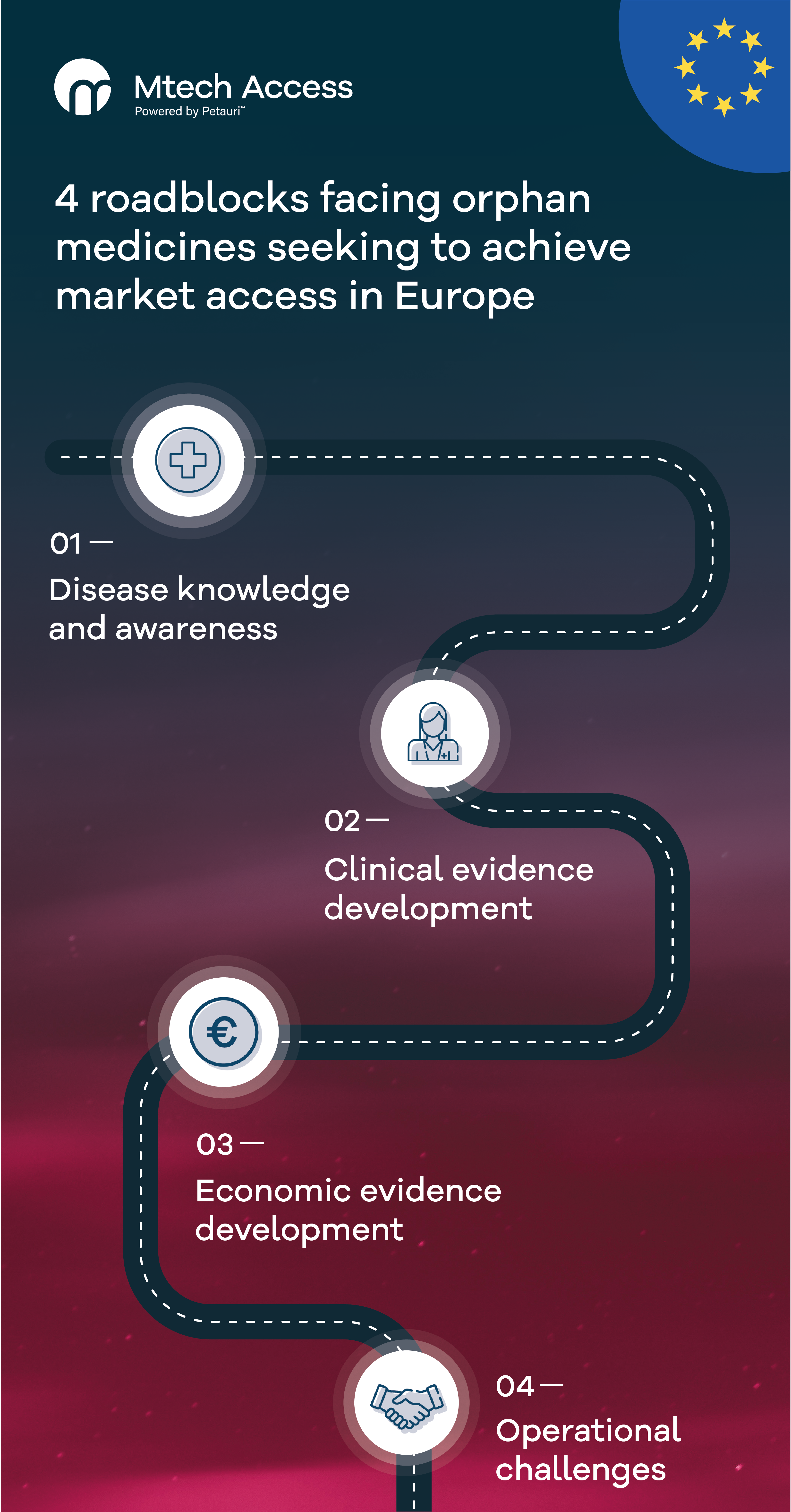
In this four-part series, we will explore the various challenges facing orphan medicines entering the European market and offer solutions that can help improve patient access. In Part 2 of the series, we will explore challenges linked to clinical evidence development. You can find Part 1 here, which explores disease knowledge and awareness.
Clinical evidence generation is a crucial stage in the market access journey for all new treatments, but can be a more significant hurdle for orphan medicines.
The characteristics of rare diseases make meeting payer evidence requirements difficult. When a non-rare disease treatment enters the market, a payer is typically presented with high quality evidence from the manufacturer, including extensive Phase 3 clinical trial data for the new treatment and comparisons with other currently available interventions. This depth of evidence is often unavailable for rare diseases.
Challenges of generating clinical evidence
Orphan drug manufacturers frequently face the following challenges when generating clinical evidence:
- Due to the small target population and the severity of most rare diseases, trial design and enrolment is challenging and far from the ideal double-blinded, comparative, parallel design of gold-standard randomised clinical trials. My colleague, Shona Lang (Director – Systematic Review), previously explored this and other related challenges in her article ‘How clinical judgement can strengthen evidence-based medicine’
- Due to the rarity and chronic nature of many of these diseases, it is often difficult to demonstrate a statistically significant impact on a mortality outcome within a randomised trial duration; thus, trials may rely on biomarkers and surrogate endpoints. For payers, this adds uncertainty around the clinical evidence, as impact on hard endpoints is key
- Rare disease indications are often heterogeneous and patients enrolled in trials may have associated co-morbidities, which, coupled with small patient numbers, further contribute to evidence generation challenges. Whilst this suboptimal level of clinical evidence is acknowledged and addressed at the regulatory level, guidance is scarce or non-existent at national and subnational payer level1
- Manufacturers looking to develop an orphan medicine or orphan device often need to address the requirements for paediatric medicines at an early stage for regulatory approval, given that many rare diseases affect children2
- Furthermore, the regulatory environment for orphan medicines is well-established, but is less mature for orphan devices. In July 2024, the European Commission published new guidance to define orphan devices and address some of the challenges faced by manufacturers of medical devices indicated for use in rare diseases3
It should be noted that some countries have adapted their reimbursement processes to recognise these differences. A recent study found that 13/32 European countries use supplemental appraisal/reimbursement processes for orphan medicines.4 These allow application of different evidence requirements and thresholds (e.g. higher incremental cost-effectiveness ratio thresholds may be accepted by the National Institute for Health and Care Excellence (NICE) when products are assessed via the highly specialised technologies route) or may lead to exemption from the health technology assessment (HTA) process in some markets (e.g. Germany) if certain criteria are met. On the other hand, where specific processes do not exist for orphan medicines, manufacturers need to understand how the general processes and requirements may challenge successful reimbursement in those countries.
From January 2028, orphan medicines will be eligible for assessment under the European Union Joint Clinical Assessment (EU JCA) process. Each member state will be required to fill out a population, intervention, comparator(s), outcome(s) (PICO) survey to allow the EU JCA committee to identify national needs. The finalised PICOs will be communicated to the manufacturer prior to the dossier submission.5 It will be extremely challenging for manufacturers to generate evidence that satisfies all the PICOs, and national HTA bodies will continue to be responsible for reimbursement decisions. My colleague, Samantha Gillard (Director – HTA), discusses this in her article ‘EU Joint clinical assessment – implications for Pharma and Medtech’.
For orphan devices, the national HTA and reimbursement environment is even less mature. The Haute Autorité de Santé (HAS) in France, NICE in England, and Gemeinsamer Bundesausschuss (G-BA) in Germany do not have specific appraisal or reimbursement processes for orphan devices, suggesting that they will be assessed under the same pathways as non-orphan medical devices
Solutions to improve clinical evidence generation for rare diseases
To improve opportunities for broad and timely access of orphan medicines and orphan devices, manufacturers need to minimise the high level of uncertainty in their clinical data. This may be achieved by:
- Identifying biomarkers and start/stop criteria to better define the patient population and treatment duration
- Applying and/or developing disease-specific patient-reported outcomes and health-related quality of life tools
- Identifying surrogate endpoints with proven clinical utility
- Designing and implementing post-launch evidence development plans and capturing real-world data
With all of these approaches, manufacturers must consider the view of all stakeholders, including policy makers, regulators, payers, clinicians, and patient advocacy organisations.
If you’d like to discuss these topics with us or hear more about how we can help you overcome your current challenges in a rare disease area, email info@mtechaccess.co.uk.
- European Medicines Agency. Guideline on Clinical Trials in Small Populations. 2006. Available from: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-trials-small-populations_en.pdf. Accessed on: November 2024
- European Medicines Agency. Paediatric Regulation. 2017. Available from: https://www.ema.europa.eu/en/human-regulatory/overview/paediatric-medicines/paediatric-regulation. Accessed on: November 2024.
- Medical Device Coordination Group. Clinical evaluation of orphan medical devices. June 2024. Available from: https://health.ec.europa.eu/document/download/daa1fc59-9d2c-4e82-878e-d6fdf12ecd1a_en?filename=mdcg_2024-10_en.pdf. Accessed on: November 2024.
- Nicod E, Whittal A, Drummond M, Facey K. Are supplemental appraisal/reimbursement processes needed for rare disease treatments? An international comparison of country approaches. Orphanet Journal of Rare Diseases. 2020;15(189):50.
- European Union. Implementing regulation (EU) 2024/1381. Available from: https://eur-lex.europa.eu/eli/reg_impl/2024/1381/oj. Accessed on: November 2024.
A version of this series was originally published in 2021. The content has been updated for re-release in 2024.






[…] Read Part 2: Clinical Evidence Development […]
[…] and anticipate and overcome hurdles posed by payers. The disease knowledge and awareness and clinical evidence development challenges described in Parts 1 and 2 of this series combine to make economic modelling in rare […]